

De Silva and coworkers have also reported that the mortality rate was not different between each group. The mortality rate was no different between the patients treated with pralidoxime or those without pralidoxime. Three of the patients who did not receive pralidoxime because of unavailability died. Two patients did not receive pralidoxime because of delayed admission and they were successfully treated with atropine alone. Thirty-two (68%) of our patients used the OP insecticide for suicide. Ingestion of OP compounds for suicidal purposes is a major problem, especially in developing countries. The duration of the intensive care stay was 5.2 ± 3.0 days. These complications were respiratory failure (14 patients), aspiration pneumonia (10 patients), urinary system infection (6 patients), convulsion (4 patients) and septic shock (1 patient). Complications were observed in 35 (74.4%) patients. Intermediate syndrome was observed in 9 (19.1%) patients. The mortality rate for the patients who required mechanical ventilation was 50%, but the rate was 21.6% for the patients who were not mechanically ventilated. Ten patients (21.2%) required mechanical ventilation. The most frequent signs were meiosis, change in mental status, hypersalivation and fasciculations. The mortality rates for the patients who did and did not receive pralidoxime were 32 and 18.7%, respectively, and were not statistically different. The gastrointestinal route was the main route in 44 (93.6%) patients.
Thirty-two (68%) were suicide attempts and 15 (32%) were accidental exposure. There were 25 female and 22 male patients. Data are presented as mean ± standard deviation. The chi-square test was used for statistical analysis. Weaning was performed using either T-tube trials or pressure support weaning. Positive end expiratory pressure was titrated to keep SaO 2 above 94% with 40% FIO 2. Mechanical ventilation was performed as synchronized intermittent mandatory ventilation + pressure support mode, either as volume or pressure control. The patients were intubated and mechanically ventilated if the patients had respiratory failure, a depressed level of consciousness, which causes an inability to protect the airway, and hemodynamic instability. Other measures for the treatment were gastric lavage and administration of activated charcoal via nasogastric tube, and cleansing the patient's body with soap and water. Pralidoxime could not be given to 16 patients: 2 patients did not receive pralidoxime because they were late admissions and 14 did not receive pralidoxime because the Ministry of Health office was out of stock. Intravenous atropine and pralidoxime was administered as soon as possible.

Diagnosis could not be confirmed with serum and red blood cell anticholinesterase levels because these are not performed at our institution. Diagnosis was performed from the history taken either from the patient or from the patient's relatives about the agent involved in the exposure. MethodsĪ retrospective study was performed on the patients with OP poisoning followed at our medical intensive care unit. We report our experience with the intensive care management of serious OP insecticide poisonings. The clinical course of OP poisoning may be quite severe and may need intensive care management. Treatment of OP poisoning consists of intravenous atropine and oximes.

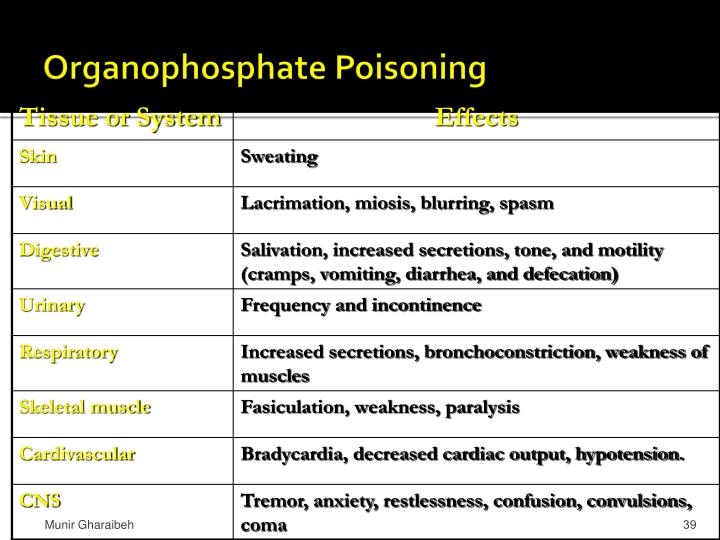
Early diagnosis and appropriate treatment is often life saving. The mortality rate of OP poisoning is high. The inhibition of acetylcholinesterase causes accumulation of acetylcholine at synapses, and overstimulation of neurotransmission occurs as a result of this accumulation. Organophosphate (OP) insecticides inhibit both cholinesterase and pseudo-cholinesterase activities.


 0 kommentar(er)
0 kommentar(er)
